Out-of-hospital cardiac arrest (OHCA) affects over 350,000 individuals in the United States, and 275,000 individuals in Europe each year. In-hospital cardiac arrest (IHCA) occurs in an estimated 290,000 patients per year in the United States. The mortality remains high for both conditions with only approximately 10% surviving OHCA and 30% surviving IHCA.
Cardiac arrest causes whole body ischemia with subsequent reperfusion injury during cardiopulmonary resuscitation (CPR) and return of spontaneous circulation (ROSC). This elicits a complex pathophysiological response that has been termed the post-cardiac arrest syndrome. In order to mitigate organ dysfunction inflicted by the post-cardiac arrest syndrome, post-resuscitation care has received considerable attention and is now incorporated into international guidelines.
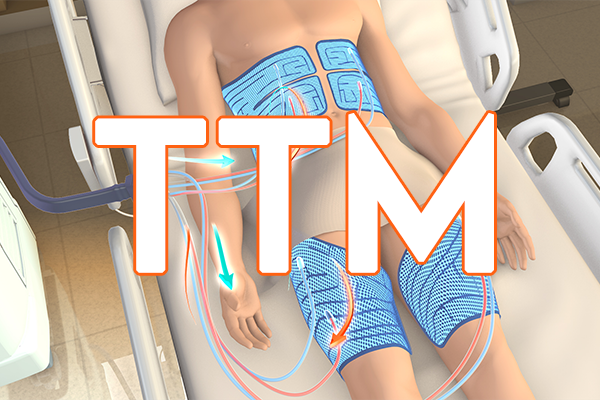
Post-resuscitation care includes therapies aimed at optimizing ventilation and circulation, preserving organ/tissue function, and reducing post-resuscitation injury. Targeted temperature management (TTM) with a target of 32– 36°C has been a mainstay of post-resuscitation care since early trials in 2002 suggested a beneficial effect after OHCA. Since then, many studies have investigated different aspects of TTM including timing, temperature targets, duration, and methods. After publication of the TTM1 trial in 2013, which did not demonstrate a benefit with a target of 33 °C compared to a target of 36 °C, there has been debate about the optimal target temperature for post–cardiac arrest patients, with new evidence available from multiple randomized trials including the large TTM2 trial. The topic was last addressed by the International Liaison Committee on Resuscitation (ILCOR) in 2021.
This course aims to review all aspects of TTM including timing, temperature, duration, method, and rewarming in order to implement current clinical practice in accordance with available evidence.